


Most patients with dry eye disease may have symptoms, but not know they have the condition. Statistics show that only 50% of patients with dry eyes have been diagnosed by an eye doctor. That means there are millions of Americans suffering out there who don’t need to be! Even fewer are being properly treated for the condition, even once diagnosed.
So where do things go wrong? It is difficult to explain, as the causes are intermingled, but it can help to think of things falling under three major categories.
We know that dry eye is a chronic, progressive, inflammatory condition. All it may take is a “lit match” to set off the forest fire. This could include trauma like eye surgery, infection, environment or just systemic illness. The figure below describes this in greater detail. By no means is this list all-inclusive!
|
Trauma |
Mechanical Injury |
Fingernails, tree branches etc. can all cause corneal abrasions |
|
Contact Lens Use |
Contact Lenses can be considered “corneal foreign bodies” |
|
|
Corneal Refractive Surgery |
When tissue is ablated from the cornea to help correct refractive error, corneal nerves are affected and dry eyes are worsened, more so in LASIK than PRK |
|
|
Ocular Surgery |
Any kind of ocular surgery can make the eye inflamed. When steroids drops are stopped, there is often a spike in dry eye symptoms. |
|
|
Periocular Surgery |
General anesthesia without taping the eyelids shut can cause a corneal abrasion that is noticed immediately upon awakening. Additionally, lid surgery can cause an exposure keratopathy |
|
|
Chemical or Thermal Injury |
This causes direct damage to cells, resulting in a rapid rise in inflammation |
|
|
Drug Allergies |
This systemic problem affects mucous membranes, potentially causing severe damage to the conjunctiva |
|
|
Infection |
Viral Conjunctivitis |
Can result in longstanding conjunctival damage |
|
Corneal Ulcer |
Chronic activation of immune system along with possibly toxic eyedrops needed for treatment |
|
|
Herpes Simplex or Shingles |
Can result in a neurotrophic keratopathy (numb cornea) |
|
|
Blepharitis |
Toxins secreted by either staph bacteria or demodex mites may activate the immune system |
|
|
Environment |
Seasonal Allergies |
Activation of immune system |
|
Computer Use |
Decreased blink rate and increased amount of incomplete blinks |
|
|
Systemic Conditions |
Diabetes Mellitus |
Can result in mild neurotrophic keratopathy (numb cornea) |
|
Thyroid Disease |
Increased risk of exposure keratopathy |
|
|
Menopause |
Hormonal changes in estrogen and progesterone cause all manner of ocular surface changes, mainly in the eyelids |
|
|
Radiation |
Destruction of the lacrimal glands if given locally around the face |
|
|
Dermatologic Diseases |
Skin conditions that cause rashes such as lichen planus, ocular cicatricial pemphigoid, pemphigus vulgaris can cause an increased immune response |
Once the process has begun, the local immune system senses damage and spreads out factors to neighboring cells, which secrete their own factors to their neighbors. This, unfortunately, spreads across the cornea and conjunctiva, eventually causing cell death. It is a vicious cycle, resulting in tear film changes at virtually all three levels. Goblet cells in the conjunctiva are lost, affecting the mucin level. Cells in the lacrimal gland die off, decreasing the amount of aqueous. Oil in the meibomian glands starts to thicken. We’ll look at that last one closely later as it is an important topic on its own.
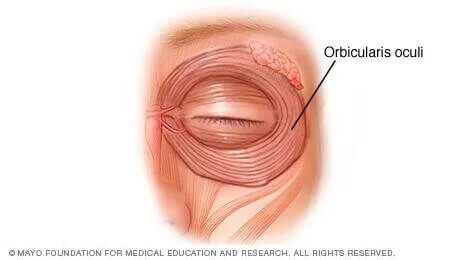
There are multiple mechanisms involved in the blinking process. One of the biggest culprits when it comes to dry eye involves the orbicularis oculi muscle. This muscle surrounds the eye and during a normal blink squeezes around the meibomian glands in the four eyelids. It exerts approximately 0.6 PSI—not a tremendous amount of pressure. We are born knowing exactly how to blink. Unfortunately, we spend a lifetime forgetting how to do so. Why? You can thank technology! Studies have shown that people blink 5 times less frequently when staring at a screen. When was the last time you were staring at a screen? You’re probably doing so right now! In addition to the frequency being reduced, the quality of the blink also suffers. The blinks become incomplete, with the upper eyelids never fully making contact with the lower eyelid margin. The problem with this is twofold.
Another ocular mechanism is how the produced tears are split 50/50 between lubrication of the ocular surface and filling of the inferior pocket or fornix of the conjunctiva. As explained previously, this reservoir of fluid can be accessed if the ocular surface is drying out and the next replenishing blink isn’t coming anytime soon. When there is chronic inflammation, as there is in dry eye, the connections that hold the conjunctiva tightly adhered to the underlying tissue start to dissolve. The conjunctiva in the pocket starts riding upwards with the seemingly loose, redundant conjunctiva sitting on top of the eyelid margin. This problem is also twofold.
At this point, you may start to realize the pathology of dry eye is all very much entwined. Let’s look at a scenario.
Scenario 1: A 50-year old female realtor who is constantly on her phone or laptop complains of dry eye symptoms. Due to her age, she may be undergoing menopause with the accompanying hormonal changes wreaking havoc on her eyelids. She’s looking at screens constantly, so her blink rate and blink quality are both diminished. The bottom part of her cornea is drying out, despite still having an adequate tear reservoir, simply because she is only blinking once every 10-12 seconds. The cells at the bottom part of the cornea start the inflammatory pathway to warn/irritate the neighboring cells and…now the dry eyes are progressing full stream ahead with no relief in sight! We see there is no solitary reason for the symptoms in this scenario. There are multiple causes all working simultaneously towards one goal—causing you discomfort and affecting your quality of life. A multifactorial approach to treatment will be needed here.
Oil Glands
Dry eye used to be divided into two major categories:

It turns out that most people cannot be pigeon-holed into one category or the other. One may start before the other, but most people suffer from a mix of both, with evaporative being the biggest contributor.
Why does the oil in meibomian glands not want to come out? We discussed earlier how a good blinking mechanism is needed to squeeze out the oil. It turns out chronic inflammation in the setting of poor, incomplete blinking results in a change in oil consistency. It becomes thicker, more viscous, and starts resembling paste or butter more than a liquid like oil. When the oil is thick, even if you squeeze your eyes hard, it won’t matter. There simply isn’t enough pressure to get it out. This may contribute to frequent styes as the problem becomes more prevalent. Eventually this “bad oil” can loiter in the meibomian glands and cause their destruction. These glands cannot be brought back once this happens. Sometimes, especially in the setting of prolonged inflammation, small membranes can grow over or inside in the meibomian glands. At first, it narrows the opening and then eventually it can close it completely. Even thinning of the oil may not help in this setting since the opening of each oil gland has been sealed.
Other factors that can contribute to the change in oil gland thickness are diet and hormones. In the American diet, the critical fatty acid ratio is:
This ratio tends to be quite low compared to our Mediterranean counterparts, since we don’t eat as much seafood. Omega-3 fatty acids are “healthy” and have an anti-inflammatory action. Omega-6 fatty acids are “not healthy” and may cause inflammation. Hormones change in both men and women as they get older, but women are particularly affected when menopause occurs (or after a hysterectomy). Women on hormone replacement therapy with estrogen and progesterone often have a resolution in their symptoms. No such benefit exists when women are only on estrogen. Since there are inherent risks of uterine and ovarian cancer with hormonal replacement therapy, it is not a popular treatment these days. We can better evaluate a patient’s oil secretion by utilizing a combination of diagnostic testing and clinical exam. We currently use the Antares for our imaging. We have patients keep each eye open and measure how long it takes before the tear film dries out on the cornea. Good areas are colored green, adequate ones are yellow and poor are colored red, for easy interpretation. Additionally, the oil glands are scanned, similar to an x-ray, but using safe infrared light, not radiation. This meibography can show areas of meibomian gland dilation (reversible) and destruction (irreversible). This helps give both patient and physician an understanding of how bad the dry eyes truly are and what level of treatment is best needed.
Level 0 meibomian gland disease (MGD) means the oil glands look perfect! Mind you, they could still be clogged but anatomically they are normal.
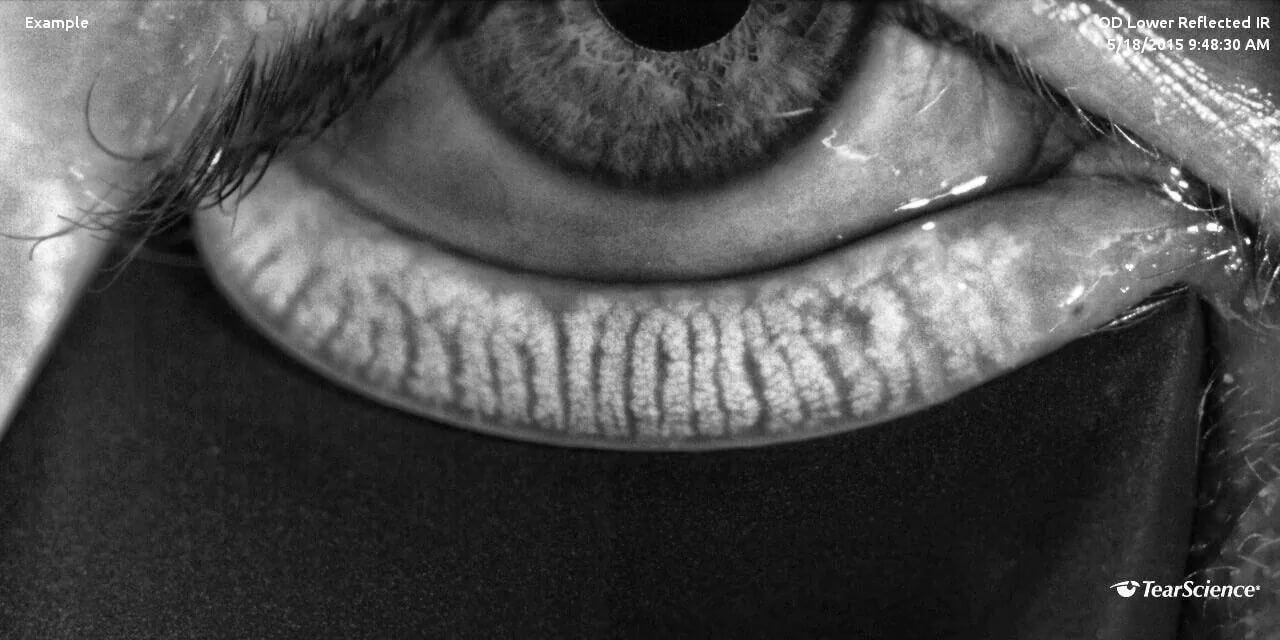
Level 1 MGD means the clogged oil has now started making the meibomian gland(s) dilate. It can be unclogged and functional, but the dilation may remain even after treatment.
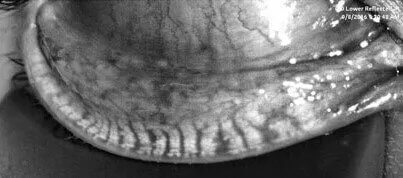
Level 2 MGD means that the “bad oil” has now started causing gland destruction. This damage is irreversible. There should be enough salvageable glands elsewhere where this can be overcome, but treatment may need to be more aggressive.

Level 3 MGD means there is a vast loss of normal oil gland architecture. Even aggressive treatment may not eliminate symptoms completely, as the damage has already been done. Supplementation with tears and other lubricants becomes more of a mainstay of treatment.
